CPR Science
One fact about CPR and other post–cardiac arrest treatments is certain: no amount of defibrillation will impact outcomes if there is no perfusion to the heart and brain. Re-establishing blood flow to the vital organs is the single most important factor for successful resuscitation, especially when the duration of cardiac arrest is prolonged beyond four minutes.
Tang et al., conducted a study with an opioid receptor agonist, noted that after induced cardiac arrest, myocardial PO2 did not fall to zero until after four minutes of non-perfusion.1 That was contradictory to traditional textbook physiology, which projects that when cardiac output ceases, the heart becomes ischemic immediately. The group was later able to show, using orthogonal polarization imaging, that the reason for this window was the time it takes until the arterial and venous pressures balance. Until they do, the red cells continue to bring oxygen to the myocardium. Beyond this window, the only means to resuscitate patients is to re-establish circulation to perfuse the myocardium.
Additional evidence for the four-minute window is found in energy stores. In order for the heart to contract, membrane potentials must be maintained, and calcium must remain sequestered in the cells. These processes are dependent upon adenosine triphosphate (ATP). As the oxygen supply is depleted, the myocardium becomes depleted of ATP, membrane potentials degrade, myocardial function decreases, and the heart gradually becomes no longer receptive to a shock after approximately four minutes of VF.
Coronary Perfusion Pressure
According to American Heart Association Guidelines for CPR and ECC, “The important pressure for perfusion of the myocardium is coronary perfusion pressure.”2
The driving force for coronary blood flow is aortic pressure less the pressure resisting flow (right atrial pressure), and this yields the blood pressure gradient for the vascular bed. Coronary perfusion pressure is therefore the difference between right arterial pressure (RAP) and aortic pressure (AoP) during diastole.
Note: Obtaining coronary perfusion pressure (CPP) is an invasive technique that measures the pressure in the coronary arteries immediately upon diastole and is used primarily for research purposes. It is neither routinely available nor practical in the resuscitation setting.
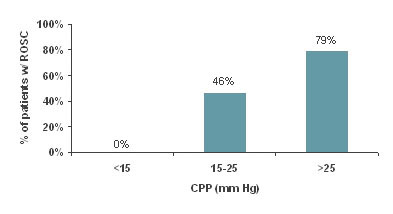
Nonetheless, CPP has tremendous clinical significance, and Paradis et al, who measured the coronary perfusion pressure of patients undergoing CPR in an ICU, demonstrated this in JAMA in 1990.3
In Paradis' study, no patient achieved return of spontaneous circulation (ROSC) with coronary perfusion pressures less than 15 mm Hg, while ROSC was achieved in 79% of those patients with a CPP greater than 25 mm Hg.
The following images show the progression of ventricular fibrillation (VF) over time and the impact of CPR on reconstituting the waveform. Initially, VF is coarse and generally still shockable. Myocytes are still contracting uniformly along a few wave fronts.
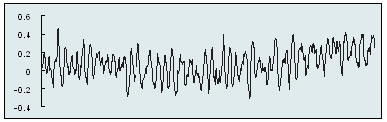
Initial VF Waveform
After five minutes, myocyte contraction is more independent, more wave fronts develop, and the ability of the heart to respond to a shock declines dramatically. This critical time can be observed by the smoothing and decreasing amplitude of the waveform.
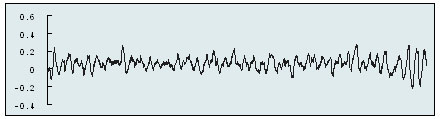
VF Waveform After Five Minutes without Effective CPR
Shown below is the waveform after three minutes of effective CPR. By providing perfusion to the heart, CPR reconstitutes the VF into the shockable coarse form.
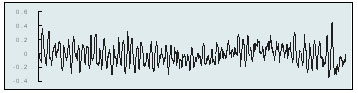
VF After Three Minutes of Effective CPR
Establishing circulation with CPR at a level fast enough and deep enough to achieve an effective CPP is therefore the goal of CPR compressions. This was clearly the goal of the changes to the 2005 AHA Guidelines for CPR and continued into 2015.
AHA 2015 Guidelines for CPR and ECC
The American Heart Association 2015 Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care emphasizes the critical importance of effectively performed CPR to resuscitation.4
The American Heart Associate defines effective CPR as:
In adult victims of cardiac arrest, it is reasonable for rescuers to perform chest compressions at a rate of 100 to 120/min (Class IIa, LOE C-LD).
- During manual CPR, rescuers should perform chest compressions at a depth of at least 2 inches or 5 cm for an average adult, while avoiding excessive chest compression depths (greater than 2.4 inches [6 cm]) (Class I, LOE C-LD). Compression depth may be difficult to judge without use of feedback devices, and identification of upper limits of compression depth may be challenging.
- In adult cardiac arrest, total preshock and postshock pauses in chest compressions should be as short as possible (Class I, LOE C-LD) because shorter pauses can be associated with greater shock success, ROSC, and, in some studies, higher survival to hospital discharge.
- In adult cardiac arrest with an unprotected airway, it may be reasonable to perform CPR with the goal of a chest compression fraction as high as possible, with a target of at least 60% (Class IIb, LOE C-LD).
The Guidelines also recommend:
- Allowing for complete chest recoil after each compression
- Minimizing interruptions in chest compressions
- Avoiding excessive ventilation
1. Tang, et al. A delta opioid receptor agonist minimizes myocardial ischemia during cardiopulmonary resuscitation. Crit Care Med. 2001;29: A18.
2. American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation supplement 2005; 112:IV-1-IV-211.
3. Paradis, et al. Coronary Perfusion Pressure and the Return of Spontaneous Circulation in Human Cardiopulmonary Resuscitation. JAMA. 1990;263(8):1106-1113.
4. Neumar, RW. Part 1: Executive Summary. 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015.