Carbon Dioxide and Oxygen
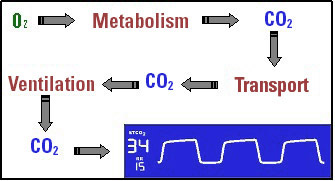
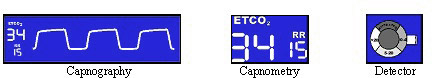
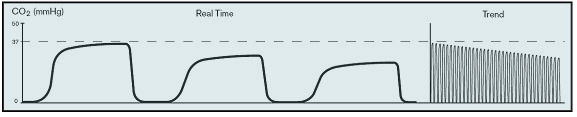
Capnography refers to the comprehensive measurement and display of CO2 including end-tidal and inspired CO2, and the CO2 waveform, which is referred to as the capnogram. Capnography depicts the three components of respiration -- metabolism, transport, and ventilation -- and therefore gives an excellent picture of the respiratory process.
A capnometer is a device that measures CO2 and displays a waveform. Capnometry refers to the measurement and display of CO2 in numeric form only and detectors are qualitative devices that indicate a range of CO2.
There are two types of sampling techniques, mainstream and sidestream, which refer to the position of the sampling device (infrared bench) relative to the source of gas being sampled. Mainstream CO2 sensors are placed at the airway of an intubated patient, allowing the inspired and expired gas to pass directly across the IR light path. The major advantages of mainstream sensors are fast response time, elimination of water traps, and crisper waveforms.
Sidestream CO2 sensors are located away from the airway, requiring a gas sample to be continuously aspirated from the breathing circuit or patient, and transported to the sensor by means of a pump. This type of system is best suited for non-intubated patients.
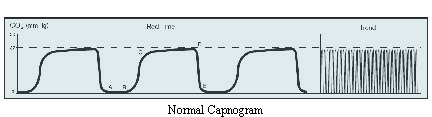
Waveform Characteristics:
| • A-B Baseline | • D End-Tidal Concentration |
| • B-C Expiratory Upstroke | • D-E Inspiration |
| • C-D Expiratory Plateau |
Physiologic factors that affect the level of EtCO2.
Increasing EtCO2:
| • Decreased minute ventilation | • Bicarbonate infusion |
| • Increased muscular activity (shivering) | • Tourniquet release |
| • Malignant hyperthermia | • Effective drug therapy for bronchospasm |
| • Increased cardiac output (during resuscitation) |
Decreasing EtCO2:
| • Increased minute ventilation | • Decreased cardiac output (cardiac arrest) |
| • Decreased muscular activity (muscle relaxants) | • Bronchospasm |
| • Pulmonary embolism |
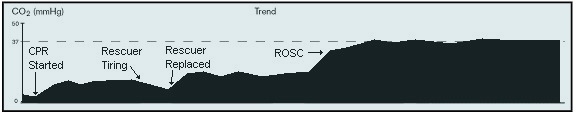
Applications during resuscitation include:
- Help confirm the correct placement of an endotracheal tube (ETT) into the trachea
- Evaluation of the effectiveness of chest compressions
- Return of spontaneous circulation
- Assessment of airway obstruction
Esophageal Intubation will either show no CO2 waveform or small transient waves.

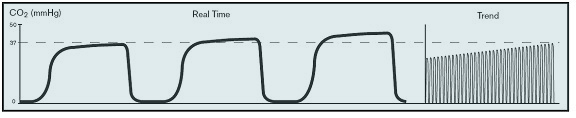
EtCO2 Trend of CPR
SpO2 – There are three primary ways to measure oxygen saturation (SaO2).
- Blood Gas Analyzer
- Co-oximeter
- Pulse Oximeter
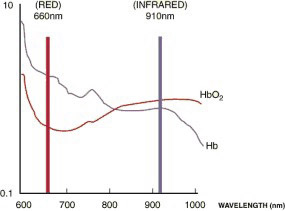
The principle of pulse oximetry is to transmit two specific wavelengths of light through a pulsating vascular bed. These wavelengths are based on the red and infrared light absorption characteristics of oxygenated and deoxygenated hemoglobin. A photodiode measures the ratio of light absorption which passes through the vascular bed.
Oxygenated hemoglobin absorbs more infrared light and allows more red light to pass through. Deoxygenated (or reduced) hemoglobin absorbs more red light and allows more infrared light to pass through. Red light is in the 600-750 nm wavelength light band. Infrared light is in the 850-1000 nm wavelength light band. This is considered “functional” oxygen saturation which identifies oxyhemoglobin and deoxyhemoglobin.
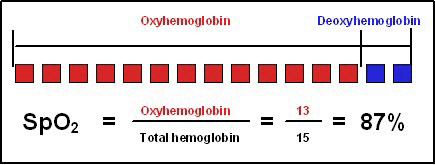
During CPR, oximetry generally will not function reliably due to low perfusion states. However, with digital technology and new processing specific for low perfusion cases the SpO2 readings have become more reliable and can indicate when return of circulation is achieved.